Delayed Gastric Emptying and Acid Reflux

Understanding the intricate relationship between delayed gastric emptying and acid reflux can transform your approach to digestive health. By delving into their connection, you can gain valuable insights that pave the way for improved management strategies.
What You Will Learn
- Delayed gastric emptying, or gastroparesis, can exacerbate acid reflux symptoms, leading to increased discomfort.
- Nerve damage, certain medications, and structural issues can cause delayed gastric emptying, affecting overall digestive health.
- Pressure build-up in the stomach from retained food can lead to heightened acid reflux activity.
- Personalized treatment strategies are essential; they should consider individual health conditions, dietary habits, and lifestyle choices.
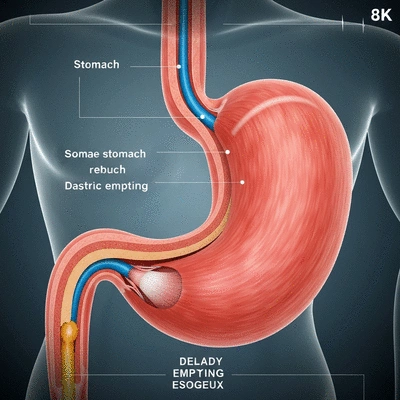
Understanding the Interplay: Delayed Gastric Emptying & Acid Reflux
The visual below illustrates the key connections and contributing factors between delayed gastric emptying and acid reflux, highlighting why addressing both is crucial for digestive health.
The Core Connection
Delayed Gastric Emptying
Food lingers longer in the stomach.
Increased Acid Reflux
Pressure builds, pushing contents into esophagus.
Factors Contributing to Delayed Emptying
Nerve Damage (e.g., Diabetes)
Certain Medications
Structural Issues/Obstructions
Impact of Impaired Gastric Motility
Reduced Contraction Frequency
Poor Muscle Coordination
The Role of the Lower Esophageal Sphincter (LES)
Healthy LES
Acts as a strong gatekeeper, preventing reflux.
Weakened LES
Allows stomach contents to flow back up easily.
Understanding Delayed Gastric Emptying in Relation to Acid Reflux
When we talk about digestive health, one term that often comes up is delayed gastric emptying, or gastroparesis. This condition occurs when the stomach takes too long to empty its contents, leading to various uncomfortable symptoms. For many of my patients at What is Acid Reflux, understanding this phenomenon is key to managing their acid reflux effectively.
In simple terms, delayed gastric emptying can contribute to feelings of fullness, bloating, and even nausea. These symptoms not only disrupt your daily life but can also worsen acid reflux issues. By shedding light on how these two conditions interact, we can start to put together a plan for better digestive health!
The Definition and Mechanisms of Delayed Gastric Emptying
Delayed gastric emptying is characterized by a slowdown in the normal movement of food from the stomach into the small intestine. This can happen due to various factors, including nerve damage, certain medications, or even underlying conditions such as diabetes. The primary mechanism involves the stomach muscles not contracting as they should, which inhibits the timely passage of food.
Research published in PubMed Central highlights the diagnostic challenges and treatment options for gastroparesis, providing further insights into this complex condition.
- Nerve Damage: Conditions like diabetes can damage the vagus nerve, which controls stomach muscles.
- Medications: Some medications, especially pain relievers and antidepressants, can slow down gastric emptying.
- Structural Issues: Blockages or obstructions in the stomach can lead to delayed emptying.
Understanding these mechanisms allows us to recognize how they may also be linked to acid reflux symptoms, as food lingering in the stomach can create more pressure and discomfort, pushing stomach contents back up into the esophagus.
Clarifying the Connection Between Delayed Gastric Emptying and Acid Reflux
The connection between delayed gastric emptying and acid reflux is a crucial aspect of digestive health. When food sits in the stomach for longer than normal, it can increase the chances of reflux, as the pressure builds up. This means that individuals experiencing delayed gastric emptying may also be more prone to the burning sensations and discomfort associated with acid reflux.
A study on gastroparesis and gastroesophageal reflux disease (GERD) in PubMed Central further supports this connection, emphasizing how delayed gastric emptying can exacerbate GERD symptoms.
- Increased Pressure: The longer food remains in the stomach, the more pressure it exerts on the lower esophageal sphincter (LES).
- Acid Production: Prolonged gastric retention can lead to increased acid production, further aggravating reflux.
- Digestive Discomfort: Symptoms like bloating and fullness can make reflux more pronounced.
Recognizing this connection is essential for developing a comprehensive management plan. By addressing delayed gastric emptying, we can often alleviate the severity of acid reflux symptoms, leading to a more comfortable lifestyle.
Examining Gastric Motility and Its Impact on Acid Reflux Symptoms
The term gastric motility refers to the movements of the digestive system that facilitate the passage of food. When gastric motility is impaired, it can lead to significant discomfort and a host of digestive issues, particularly concerning acid reflux. I often tell my patients that understanding their body's motility patterns is vital in managing their symptoms.
- Frequency of Contractions: Healthy gastric motility involves regular contractions that push food through the digestive system.
- Coordination: Proper coordination between stomach muscles and the digestive tract is essential for efficient functioning.
- Symptom Awareness: Recognizing the signs of poor gastric motility can help in seeking appropriate treatment.
By focusing on gastric motility, we can better address the underlying issues that contribute to both delayed gastric emptying and acid reflux. It’s about creating a dialogue between your body and mind to improve your overall digestive well-being.
Pro Tip
To effectively manage both delayed gastric emptying and acid reflux, consider keeping a food diary. Tracking your meals can help you identify specific foods that may trigger symptoms, allowing for more personalized dietary adjustments. Remember, small changes in your eating habits can lead to significant improvements in your digestive health!
Summarizing the Interplay Between Delayed Gastric Emptying and Acid Reflux
Understanding the relationship between delayed gastric emptying and acid reflux is crucial for effective treatment. Delayed gastric emptying, also known as gastroparesis, can contribute to the severity of acid reflux symptoms. When food takes longer to move from the stomach to the intestines, it can lead to increased pressure and discomfort. This interplay can make it challenging to manage digestive health effectively.

In my practice at What is Acid Reflux, I often emphasize the importance of personalized treatment strategies. Each patient's experience with acid reflux is unique, and understanding how delayed gastric emptying factors into their symptoms can lead to more tailored and effective management plans.
The Importance of Personalized Treatment Strategies
Adopting a one-size-fits-all approach to managing acid reflux is not effective. Instead, it’s essential to consider various factors, including individual health conditions, dietary habits, and lifestyle choices. Here are a few key aspects to include in personalized treatment plans:
- Assessment of gastric motility and its effect on symptoms
- Evaluation of dietary triggers specific to each patient
- Incorporation of stress management techniques
- Monitoring medication interactions that may affect gastric emptying
By focusing on these aspects, I can help patients create a roadmap toward better digestive health and symptom relief. It’s about establishing a plan that resonates with their lifestyle and addresses their unique challenges.
Understanding the Role of the Lower Esophageal Sphincter (LES) in Acid Reflux
The lower esophageal sphincter (LES) plays a pivotal role in preventing acid reflux. It acts as a gatekeeper between the esophagus and the stomach, ensuring that stomach contents don’t flow back up. However, if the LES is weakened or relaxes inappropriately, it can lead to increased acid exposure and discomfort.
Research available via PubMed provides further insights into the mechanisms and therapeutic targets for LES dysfunction, which is highly relevant to managing acid reflux.
Part of my work involves educating patients on how to support their LES function. Here are some strategies that can strengthen the LES:
- Avoiding large meals that put pressure on the sphincter
- Upholding a healthy weight to reduce abdominal pressure
- Steering clear of foods and drinks that relax the LES, such as caffeine and alcohol
Through these practical tips, we can work together to promote better acid control and improve overall digestive comfort.
Taking Action: Tips for Managing Acid Reflux and Delayed Gastric Emptying
Now that we’ve explored the connections between delayed gastric emptying and acid reflux, it's essential to take actionable steps toward better management. Here, I’ll share some tips that I've found effective in my practice for managing these issues simultaneously.
Consulting Healthcare Professionals for Tailored Solutions
It’s vital to consult healthcare professionals, like your gastroenterologist, when dealing with complex digestive issues. At What is Acid Reflux, I encourage patients to seek tailored solutions that fit their specific symptoms and lifestyle. A thorough evaluation can lead to the most appropriate treatment options, ensuring you're on the right path to relief.
Resources for Ongoing Support and Education
Education is empowering! I recommend utilizing various resources for ongoing support in managing acid reflux and gastric emptying issues. Some valuable resources include:
- Online forums and communities for sharing experiences
- Educational websites, like What is Acid Reflux, for in-depth articles and tips
- Support groups that connect you with others facing similar challenges
Engaging with these resources can provide you with insights and encouragement as you navigate your digestive health journey.
Utilizing Nutritional Interventions and Dietary Fiber for Better Management
Nutritional interventions can play a significant role in managing both acid reflux and delayed gastric emptying. Incorporating more dietary fiber can enhance digestion and help maintain a healthy weight. Here are some fiber-rich foods that I often recommend:
- Fruits like apples, bananas, and berries
- Vegetables such as leafy greens, carrots, and broccoli
- Whole grains like oats, quinoa, and brown rice
By integrating these foods into your diet, you can support your digestive health and reduce the risk of reflux symptoms. Remember, making small changes can lead to significant improvements over time!
Recap of Key Points
Here is a quick recap of the important points discussed in the article:
- Delayed Gastric Emptying: This condition slows down the movement of food from the stomach to the small intestine, leading to symptoms like fullness and nausea.
- Connection to Acid Reflux: Food lingering in the stomach can increase pressure on the lower esophageal sphincter (LES), exacerbating acid reflux symptoms.
- Importance of Gastric Motility: Healthy gastric motility involves proper contractions and coordination, which are vital for preventing digestive discomfort.
- Personalized Treatment Strategies: Tailored approaches considering individual health conditions, dietary habits, and stress management are crucial for effective management.
- Lower Esophageal Sphincter (LES) Support: Strategies to strengthen the LES include avoiding large meals and certain trigger foods like caffeine and alcohol.
Frequently Asked Questions (FAQs)
- What is delayed gastric emptying (gastroparesis)?
- Delayed gastric emptying, or gastroparesis, is a condition where the stomach takes too long to empty its contents into the small intestine. This slowdown can cause symptoms like bloating, fullness, and nausea.
- How does delayed gastric emptying contribute to acid reflux?
- When food remains in the stomach for an extended period, it increases pressure within the stomach. This elevated pressure can push stomach contents, including acid, back up into the esophagus, leading to or worsening acid reflux symptoms.
- What are the main causes of delayed gastric emptying?
- Key causes include nerve damage (often seen in conditions like diabetes affecting the vagus nerve), certain medications (such as pain relievers and antidepressants), and structural issues or obstructions in the stomach.
- What is gastric motility and why is it important for digestive health?
- Gastric motility refers to the muscle contractions that move food through the digestive system. Healthy motility involves regular and coordinated contractions, which are essential for efficient digestion and preventing issues like delayed gastric emptying and acid reflux.
- How does the Lower Esophageal Sphincter (LES) relate to acid reflux?
- The LES acts as a valve between the esophagus and the stomach, preventing stomach contents from flowing back up. If the LES is weakened or relaxes inappropriately, it can allow stomach acid to reflux into the esophagus, causing discomfort.
- What strategies can help manage both delayed gastric emptying and acid reflux?
- Effective strategies include personalized treatment plans from healthcare professionals, dietary adjustments (like incorporating fiber-rich foods and avoiding trigger foods), maintaining a healthy weight, and avoiding large meals that put pressure on the LES.