Nighttime Acid Reflux Solutions

When it comes to nighttime acid reflux, understanding the triggers and effective management strategies can drastically improve your quality of sleep. This guide will illuminate the path to a more restful night and a healthier tomorrow.
What You Will Learn
- The mechanics of acid reflux and how it disrupts sleep.
- Common triggers for nighttime symptoms, including certain foods and drinking habits.
- The strong connection between obesity and increased risk of nighttime reflux.
- Effective lifestyle changes, such as elevating your head while sleeping, to minimize symptoms.
- Immediate relief strategies to employ during nighttime episodes.
- When to seek professional help for persistent or severe symptoms.
Key Strategies for Managing Nighttime Acid Reflux
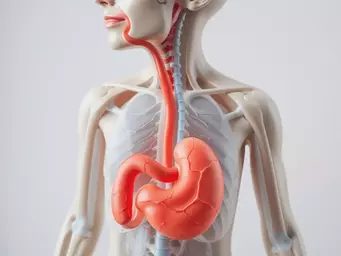
The following visual summarizes actionable tips, triggers, and medical approaches to effectively manage nighttime acid reflux, promoting better sleep and overall well-being.
Actionable Tips for Immediate Relief
• Water by bedside: Sip for discomfort.
• Chew gum: After meals to neutralize acid.
• OTC antacids: For quick relief.
• Deep breathing: To relax body & mind.
Common Triggers to Avoid
- • Heavy/fatty meals
- • Spicy/acidic foods
- • Caffeinated beverages
- • Alcohol consumption
- • Eating too close to bedtime
Key Lifestyle Adjustments
- • Elevate head while sleeping
- • Sleep on left side
- • Avoid late-night snacks
- • Limit trigger foods/drinks
- • Maintain a healthy weight
When to Consult a Professional
- • Symptoms > Twice/week
- • Difficulty swallowing
- • Unexplained weight loss
- • Signs of bleeding
Medication Overview
- • Antacids: Quick relief, neutralizes acid.
- • H2 Blockers: Reduce acid production.
- • PPIs: Long-term acid blocking.
Understanding Nighttime Acid Reflux and Its Causes
Many people experience nighttime acid reflux, a condition that can significantly disrupt sleep and overall well-being. This discomfort often stems from a complex interaction of our body’s anatomy and lifestyle choices. In this section, we will explore how acid reflux affects sleep, identify common triggers, and delve into the relationship between obesity and nighttime symptoms.
Understanding the mechanics of acid reflux is crucial for managing it effectively. When we lie down, the gravitational pull that helps keep stomach contents in place is diminished, making it easier for acid to flow back into the esophagus. This backflow can lead to a burning sensation, commonly known as heartburn, which can interrupt our nightly rest.
The Anatomy of Acid Reflux: How It Affects Sleep
Acid reflux occurs when the lower esophageal sphincter (LES) fails to close properly, allowing stomach acid to escape into the esophagus. This is particularly problematic during sleep, as lying down can exacerbate the issue. Understanding this mechanism helps us recognize why we often wake up in discomfort during the night. The National Center for Biotechnology Information provides further insights into the mechanisms of gastroesophageal reflux disease.
- The LES relaxes when we sleep, making reflux more likely.
- Sleep position can influence the severity of symptoms.
- Proper diagnosis and treatment are essential for long-term relief.
Furthermore, nighttime acid reflux can lead to a cycle of poor sleep and increased stress, which may worsen digestive issues. Learning more about how this condition operates allows us to take informed steps toward improvement.
Common Triggers for Nighttime Heartburn Symptoms
Several lifestyle factors can trigger nighttime acid reflux, making it essential to identify and avoid them. Some of the most common culprits include:
- Heavy or fatty meals
- Spicy or acidic foods
- Caffeinated beverages
- Alcohol consumption
- Eating too close to bedtime
By being aware of these triggers, we can make better dietary choices, especially in the hours leading up to sleep. Keeping a food diary can be a helpful tool in this process. It not only aids in tracking your diet but also serves as a valuable resource to discuss with your healthcare provider.
The Link Between Obesity and Nighttime Acid Reflux
Research indicates a strong connection between obesity and the frequency of nighttime acid reflux symptoms. Extra weight, particularly around the abdomen, can increase pressure on the stomach, pushing acid into the esophagus more easily. This is why maintaining a healthy weight is vital for managing acid reflux effectively. A study published in Exploration of Medicine highlights the significant impact of obesity on GERD.
- Obesity increases the risk of GERD (Gastroesophageal Reflux Disease).
- Even modest weight loss can lead to significant symptom improvement.
- Involving a healthcare professional can ensure a safe and effective weight loss plan.
How Weight Loss Can Improve Sleep Quality
Losing weight not only helps reduce acid reflux symptoms but also promotes better sleep quality. As we shed pounds, the pressure on our stomach and esophagus decreases, leading to fewer episodes of reflux. The National Center for Biotechnology Information delves deeper into the relationship between obesity and sleep disorders.
Moreover, good sleep hygiene combined with a healthy weight can enhance overall well-being. Remember, every little change counts, and taking these steps can foster a more restful night!
Understanding Gastroesophageal Reflux Disease (GERD)
GERD is a more severe, chronic form of acid reflux that can significantly affect sleep and daily life. If you experience frequent nighttime symptoms, you might be dealing with GERD. This condition not only affects the esophagus but may also lead to complications like respiratory issues or esophagitis.
Identifying GERD requires a thorough evaluation by a healthcare professional. Don’t hesitate to reach out for support—addressing these concerns early can lead to better health outcomes and a more peaceful night’s rest.
Pro Tip
Did you know? Keeping a food diary can be an invaluable tool in managing your nighttime acid reflux. By tracking what you eat and when, you can identify specific trigger foods that exacerbate your symptoms. This insight not only aids in avoiding these culprits but also serves as a constructive discussion point with your healthcare provider for tailored advice!
Summarizing Key Strategies for Managing Nighttime Acid Reflux
As we navigate the challenges of managing nighttime acid reflux, it’s important to have a few effective strategies at our disposal. These can help not just in reducing symptoms but also in enhancing our overall quality of sleep. Below, I’ve compiled actionable tips and insights that can make a significant difference in your nighttime comfort.
- Elevate your head while sleeping to prevent reflux.
- Sleep on your left side to minimize symptoms.
- Avoid late-night snacks, focusing on lighter meals.
- Limit known trigger foods and beverages before bedtime.
These straightforward adjustments can help you regain control over your sleep patterns and feel more rested each morning. Incorporating these tips into your routine can lead to a more comfortable and restorative sleep experience!
Actionable Tips for Immediate Relief
When nighttime symptoms strike, having immediate relief strategies can be a game changer. Here are some of my favorite quick fixes:
- Keep a glass of water by your bedside to sip on if you wake up feeling discomfort.
- Try chewing gum after meals; it can help neutralize stomach acid.
- Consider over-the-counter antacids for quick symptom relief.
- Practice deep breathing exercises to relax your body and mind.
Remember, these tips can provide temporary relief, but they should be part of a broader strategy for managing your acid reflux over the long term.
When to Consult a Healthcare Professional for Further Guidance
Knowing when to seek professional advice is crucial for your digestive health. If you find that your nighttime acid reflux is persistent or worsening, it may be time to reach out to a healthcare professional. Look out for:
- Symptom frequency exceeding twice a week.
- Difficulty swallowing or food getting stuck.
- Unexplained weight loss.
- Signs of bleeding, such as blood in stool or vomit.
Addressing these concerns early can lead to more effective management and better outcomes. Don't hesitate to reach out—your health is worth it!
Understanding Medications: Antacids, H2 Blockers, and Proton Pump Inhibitors
In addition to lifestyle changes, medications play a critical role in managing nighttime acid reflux. Here’s a brief overview of the most common medications:
- Antacids: Provide quick relief by neutralizing stomach acid.
- H2 Blockers: Reduce the amount of acid your stomach produces.
- Proton Pump Inhibitors (PPIs): Offer longer-term relief by blocking acid production.
Understanding these options can empower you to have informed discussions with your healthcare provider. They can help determine the best course of action tailored specifically to your needs.
Encouraging Self-Advocacy and Personalized Treatment Plans
Taking charge of your health is essential when managing acid reflux. At What is Acid Reflux, we believe in empowering you with knowledge and strategies to advocate for your health effectively!
Exploring Options Beyond Sleep Positions: Medications and Natural Remedies
While adjusting your sleep position is vital, don't overlook other treatment avenues. Here are some options you might consider:
- Explore herbal teas like ginger or chamomile that may soothe your stomach.
- Discuss with your doctor about trying probiotics for digestive support.
- Consider acupuncture or yoga as complementary therapies for relaxation.
These alternatives can complement your existing strategies and enhance your overall well-being.
Sharing Your Experiences: The Value of Community Support
Connecting with others who understand what you're going through can be incredibly beneficial. Sharing your experiences can:
- Help you discover new coping strategies.
- Provide emotional support during tough times.
- Encourage accountability in maintaining your health goals.
Don't hesitate to seek out community forums or local support groups where you can exchange tips and encouragement!
Building a Nighttime Routine for Better Digestive Health
Creating a consistent nighttime routine can greatly improve your chances of restful sleep. Consider integrating these practices:
- Establish a relaxing pre-sleep ritual, suchs as reading or meditating.
- Stick to a regular sleep schedule, going to bed and waking up at the same time daily.
- Avoid screens at least an hour before bed to reduce blue light exposure.
These simple changes can lead to a more balanced routine that supports your digestive health and helps in managing nighttime acid reflux effectively.
Frequently Asked Questions (FAQs)
- What is nighttime acid reflux? Nighttime acid reflux occurs when stomach acid flows back into the esophagus while you are lying down, often disrupting sleep due to discomfort like heartburn.
- Why is nighttime acid reflux worse than daytime reflux? When lying down, gravity no longer helps keep stomach contents in place, making it easier for acid to reflux into the esophagus and cause symptoms.
- What are common triggers for nighttime acid reflux? Common triggers include heavy or fatty meals, spicy or acidic foods, caffeinated beverages, alcohol consumption, and eating too close to bedtime.
- How does obesity affect nighttime acid reflux? Extra weight, especially around the abdomen, increases pressure on the stomach, which can force acid into the esophagus more easily, exacerbating reflux symptoms.
- What immediate relief strategies can I use for nighttime reflux? Immediate relief strategies include sipping water, chewing gum after meals, taking over-the-counter antacids, and practicing deep breathing exercises.
- When should I consult a healthcare professional for acid reflux? You should consult a healthcare professional if your symptoms occur more than twice a week, you experience difficulty swallowing, unexplained weight loss, or signs of bleeding.
- What are the main types of medications for acid reflux? The main types of medications include antacids for quick relief, H2 blockers to reduce acid production, and Proton Pump Inhibitors (PPIs) for long-term acid blocking.
- Can lifestyle changes really help manage nighttime acid reflux? Yes, lifestyle changes such as elevating your head while sleeping, avoiding late-night meals, limiting trigger foods, and maintaining a healthy weight can significantly reduce symptoms.
Recap of Key Points
Here is a quick recap of the important points discussed in the article:
- Nighttime acid reflux can disrupt sleep due to the relaxation of the lower esophageal sphincter (LES) when lying down.
- Common triggers include heavy meals, spicy foods, caffeine, alcohol, and eating too close to bedtime.
- Obesity is linked to increased nighttime reflux symptoms; even modest weight loss can lead to significant improvements.
- Effective management strategies include elevating the head during sleep, avoiding late-night snacks, and limiting known triggers.
- Consult a healthcare professional if symptoms persist or worsen, particularly if they occur more than twice a week.